How we made our podcast about the malaria vaccine
We thought we were making a documentary. We didn't realise it was also making us.
You’re reading Fix The News, a weekly roundup of stories of progress. You can subscribe or upgrade here. We give away 30% of our subscriber fees to charity. Listen to our podcast. If you need to unsubscribe, there’s a link at the end.
🎙️ A Shot At History
Apple | Spotify | Amazon
In early January 2024, I was sitting on the couch watching Netflix with my son Darcy when the phone buzzed. It was a message from Gus, my editor at Fix The News. “Listen to this” it said, with a link to a podcast episode called ‘The Call’ from This American Life. He’d found it on an annual Best Of list; it had been universally praised by podcast nerds as the best hour of audio of the previous year.
From the moment I plugged in my headphones, I was hooked. It was about a drug support hotline in the United States, and featured a single call between a user and a counsellor that unfolded into something much, much larger. It was narrative audio at its best - an intimate, personal story that said more in 60 minutes about a complex issue than a hundred articles.
At the time, we were in the middle of the second season of our own podcast, discovering for ourselves how the format allows you to tell stories that writing can’t. After a few voice memos back and forth, Gus and I promised each other that if we ever had the resources, we’d make a podcast about the malaria vaccine.
Be careful what you wish for
Two months later, we got an email from The Postcode Lottery Group in the Netherlands, one of the largest charitable funders in Europe. There was a crossover with the work they were doing and the stories we were reporting at Fix The News, and they wanted to buy an institutional subscription for their staff. Suddenly, we had the funds to make good on our agreement.
Why choose malaria? Well, it’s one of humanity’s oldest enemies. We’ve been battling it since before the invention of writing. Although it’s been eliminated in most of parts of the world, in sub-Saharan Africa, it still kills 1,000 kids every day. But now, for the first time ever, a vaccine could change that. It’s the very definition of hidden progress - a world-changing development that’s mostly invisible in the news, except for the odd occasion when it makes headlines for a day before slipping back into obscurity.
This would be our first ever attempt at something like this, so we wanted to get it right. We’re a tiny team, and making a narrative podcast was way outside our remit, so we started shopping around for experts to help us produce it. It had to be compelling. The series couldn’t feel educational or worthy, like eating your vegetables. The pitch was simple. We told everyone we wanted to make a true crime drama, except about a vaccine, not a murder.
By July 2024 we’d found a production company in Sydney that was willing to take on the challenge. The obstacles were daunting. A three part series, made remotely about something happening on another continent, with time-zone gaps, cultural differences, patchy internet, and a maze of red tape surrounding the organisations responsible for the rollout. With no budget to send a producer to Africa, we needed someone local to be our eyes and ears.
I immediately thought of my friend Barbara Gruber from Deutsche Welle. We’d been neighbours during Sydney’s lockdowns, and I remembered her working late nights on a program training storytellers across Africa to use podcasting for health communication. Now back in Berlin, she offered to spread the word through her networks, and that’s how we found the star of our show.
Ten simple words
Teresa Chirwa-Ndanga is a Malawian journalist who’s experienced malaria from every angle – as a local news director, as a child and as a mother – and on the day of our first meeting on Zoom, her mother was sick with it. As soon as she appeared, her presence filled the screen, and within a few minutes of conversation, she said something that became the through-line for the entire series.
Learning to live with a problem is not a solution.
In our years of reading everything we could about the malaria vaccine, we’d saved hundreds of thousands of words in articles, reports and emails. But there was something about the combination of those ten words that cut to the heart of this story. The science, the statistics, the history, the people - all of it could be wrapped around this single guiding principle, showing how deeply this disease has woven itself into daily life across sub-Saharan Africa.
The production company saw something there too. After the call, they suggested we engage Teresa not as a producer but as a co-host with Gus. On paper it was perfect. They were same age, both had young daughters and had grown up in different African countries, but with vastly different experiences of malaria. He could explain why it mattered; she could show what it meant on the ground. It felt like things were off to a good start.
“Something’s missing”
Given the scale of the story, we made a decision to narrow the focus to one country: Sierra Leone. Our producer was relentless, in the best possible way. He chased every lead, jumped on calls at obscene hours, and recorded the interviews on Whatsapp when the internet collapsed. His biggest breakthrough came when he managed to tap into the country’s Kombra Network, a coalition of religious leaders, young people and concerned women educating their communities about malaria.
The coolest 12 year old in Sierra Leone
In the background though, the clock was ticking. The production company had other projects in the pipeline which meant we had a limited window to get the series done. Although the interviews were going well, we noticed the conversations were increasingly being steered towards the issue of hesitancy. For most media organisations, that’s the default angle for a vaccine story (just take a look at the headlines right now) but we knew it wasn’t the approach we wanted.
We also sensed that something was missing. While malaria is primarily an African problem, the development of the vaccine was global – and that meant we needed a voice to tell us what it all meant on the world stage. I hustled to connect with a senior person at one of the big global health players. Despite hours of internet sleuthing and dozens of carefully crafted emails to WHO, Gavi and UNICEF, by the end of 2024 I’d only made minor inroads.
The power of partnerships
In January 2025, I was on a Zoom call with the Clinton Foundation when they asked what we were working on. I mentioned the documentary, and how we were struggling to find someone to talk to at the highest level. They offered to connect us with a few people, and within days we were speaking with Dr Mary Hamel, the Team Lead for Malaria Vaccines at the WHO, and someone who has spent more than three decades in this fight.
Mary describes her first experience of seeing malaria
As we wrapped the interview, we asked Mary who else we should speak to, and she immediately gave us the name of Dr Joe Cohen. Despite all our reading, we’d never heard of him, yet he turned out to be a crucial piece of the puzzle - the scientist who cracked the code of the vaccine. His story was remarkable. In the 1980s he’d spent years working weekends and late nights in his lab at what is now called GlaxoSmithKline, eventually making the breakthrough that outsmarted the parasite that had defeated generations of researchers.
Mary also connected us with Dr Mehreen Datoo, who ran the early clinical trials for Oxford’s R21 vaccine. For us, these were two versions of the same breakthrough - different labs, slightly different approaches, but ultimately part of the same historic step forward. We were feeling quietly satisfied, and thought we were getting close to a good ending. But as we were piecing the science together, the global headwinds were changing direction.
One stubborn scientist, tinkering away in a lab
Things fall apart
By February 2025, as we were wrapping our final interviews, the world looked very different to the one we had started production in seven months earlier. USAID had, shockingly, been destroyed by Elon Musk, and the United States had withdrawn from the World Health Organisation. Multilateralism suddenly felt like a relic, global health itself was under siege.
We jumped on a call with Dr Scott Gordon, who leads the Malaria Vaccine Programme for Gavi, one of the organisations pivotal to the vaccine rollout. From the headlines we assumed that they were fighting an uphill battle. Scott didn’t downplay that - funding was precarious, the challenges were real. But he also shared something we hadn’t heard: signs of real change were emerging on the ground. He told us about Kisumu, Kenya, one of the first target regions, where the children’s wards in local hospitals were beginning to empty out.
It’s working
Just a week earlier, Mary Hamel had described working in Kenya in the 1990s, when malaria had been so widespread, and so virulent, that children would die in line waiting to be seen. Now there were empty beds. Two stark, unforgettable images, and proof that something had shifted. What Scott had told us didn’t appear in any of the formal reports; it was anecdotal, fragile, early. But it was also proof that this entire effort - the decades of research, the logistics, the money, the faith - was actually saving lives.
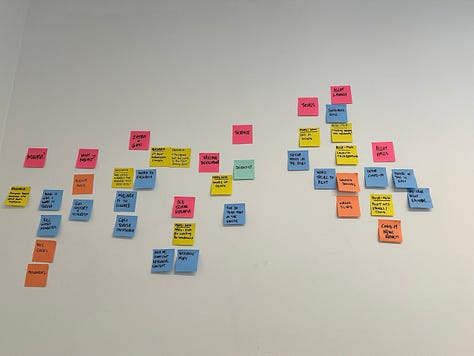
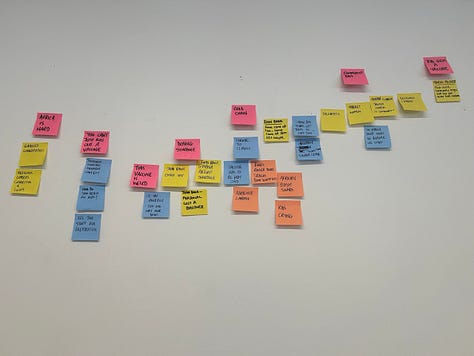
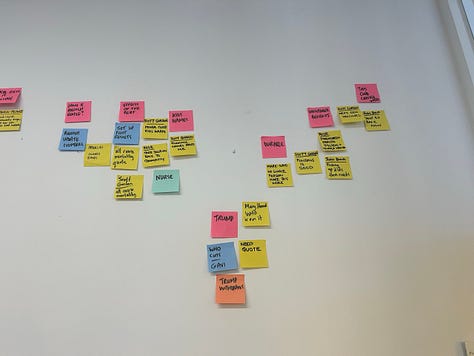
As the story shifted under our feet it was clear that the series could no longer live inside the borders of Sierra Leone. We had to go back to the production company with a new plan. I flew to Melbourne, where Gus and I spent eight hours inside a meeting room, and re-mapped the entire series from scratch with Post-It notes on the wall.
Mind the gap
March and April were a blur. The production company was sending us draft scripts, we were giving feedback, Gus and Teresa started recording the narration. We were all furiously trying to match up the story we started with to the one that was evolving in real-time.
In mid-May, the final edits of all three episodes landed in our inbox. It was a Monday morning; I’d just dropped Darcy to school, and started listening on my walk home. My stomach dropped. In creative work it’s called ‘the gap’ – the uncomfortable disconnect between your vision and the final delivery. It can be hard to pin down, but often it’s less about content and more about resonance.
The first episode opened with an intimate monologue from Gus, hours after the birth of his daughter. Although Teresa was there as the co-host, when she said “learning to live with the problem is a not a solution” the words didn’t land in the same way. The balance was way off. It wasn’t about right or wrong. There were a hundred ways to tell this story. But when we listened to that edit we realised it wasn’t our way of telling it. And once we knew that, we couldn’t un-know it. We needed to make a choice.
Going rogue
We were out of runway. The production company needed to move on and we didn’t have any more money. So we called it: we’d take the raw audio files and remake the entire series ourselves, in-house. It meant starting over with zero narrative production experience and running the risk of wasting all the interviews, all the trust people had given us. Commercially, it was a disaster.
Except, Fix The News is not a commercial media organisation. There were no KPIs or network bosses involved, there was no release date that we needed to hit. If there was ever a good argument for independent, subscriber-funded media, this was it. Backing out wasn’t an option, because we felt like we had an unspoken contract with this story. From all our conversations, the fact this vaccine reached even one kid, let alone millions, felt like a miracle.
We also held precious details from the people we’d spoken to: Salamatu, the young health club champion in Sierra Leone who wanted the world to know about malaria to help her family; Amanda the healthcare worker who slept in her car when she travelled to remote villages; Dr Rose, who was tasked with organising the pilot program in Kenya just days after starting a new job at the Ministry of Health. These were small but important fragments that might never reach a global audience.
This was our shot to tell a story that we deeply cared about. To shine a light on a disease that is just a word for people in rich countries, but devastates daily life for hundreds of millions across an entire continent. It was also a story about incremental change and unglamorous persistence - exactly the kind of thing that never makes the news, yet is almost always what actually changes the world. Basically, everything that makes solutions journalism such a tough gig.
The chain
Another shot at history
The next few weeks were a rollercoaster. The initial high of making a crazy decision quickly gave way to grinding reality. There was still a newsletter to publish, the fourth season of our other podcast was in full swing, and life outside Fix The News kept moving with all its usual chaos.
My roots are in commercial television, and the unexpected irony is that I couldn’t have taken on A Shot At History if I hadn’t earned my stripes on shows like Australia’s Next Top Model. I dusted off the old toolkit and called Anthony Badolato, our amazing sound engineer. He shares a similar background to me, except in commercial radio, and while he was eager to help, the series needed to fit around his full time job.
It was obvious we needed a different approach. Where the first version had been tightly scripted and heavily produced, we decided this one needed to feel more casual, more personal. I reached out to Teresa and set up a group call for her and Gus, to see what they’d both learned through the interviews. There was no pressure, no agenda. But Anthony and I hit record just in case - and lucky we did, because that conversation became the backbone of the entire series.
It was a Saturday afternoon when the four of us logged on. Teresa told us about her first encounter with malaria in rural Malawi, and how the disease impacted everything from farming to female leadership. Gus spoke about his long obsession with the vaccine and how he’d grown up with an ambient awareness of the disease, but had never suffered from it directly. An hour into the call, Teresa described holding her baby as she was burning up from malaria. It was tender and raw, and utterly heartbreaking. Immediately we knew we had our opening hook, and a reframe.
This had never been a story about hesitancy. It was a story about mothers. They’re the ones who carry sick children to clinics in the middle of the night, who decide whether to trust a new vaccine, who show up for trials without guarantees, who hold the line when everyone else is afraid of the unknown. They’re not passive recipients of public health interventions. They’re the decision-makers, taking risks the rest of the world will never see. And once we realised that, the rest fell into place.
It’s all about the mothers
Off we go… again
From the first week of June until the last week of September, we lived and breathed this podcast. There were no weekends, our phones vibrated with late night anxieties and early morning revelations. We talked to each other more than our families. I quickly learned how to use the editing software Descript, and scanned through every recorded interview; digging until I found the most important moments of connection.
I arranged and rearranged the puzzle pieces of the story, constantly balancing the need for information versus emotion. Anthony’s sound design reached a whole new level – as did his Youtube search history. He spent hours every night sourcing the sounds of stove burners in rural Uganda, a particular vehicle off-roading in Sierra Leone, or the busy corridors of a hospital in urban Malawi. He kept coming back to one word - authentic. If we couldn’t be physically on the ground in Africa, he was determined to at least transport our ears there.
Anthony works his magic
The biggest shift in the new version though, was Teresa’s role. I decided to put her front and centre as our guide for the series. Gus was still there as a narrator, but everything we explored was filtered back through Teresa’s experience. I remember one moment, when she learned about the scientists who worked on the vaccine. For most of her life Teresa said she felt like Africa had been abandoned by the rest of the world. Knowing the names of people who had dedicated everything to solving this problem gently changed that view.
The process was like driving at night; I could only see as far as the headlights reached. But what kept me going was a shared belief that this story wanted to exist in the world and that I needed to trust it and step out of its way. The flywheel spun hard during those months, but when you’re speaking to people who have lost loved ones and dedicated their lives to ending a disease, going all-in on a podcast doesn’t feel like such a big deal.
This is angelic
The strangest moment came when the documentary reached back into the real world, and I found myself at a table surrounded by malaria scientists in New York. I’d travelled there in late September for the UN General Assembly and Climate Week, and for the first five days, didn’t leave my friend’s apartment – I was editing the final episode during daylight and jumping on video calls at night to handover to Teresa, Gus and Anthony. Across two time zones, we were working on it 24/7.
A few days after landing I was invited to a lunch hosted by the Gates Foundation to celebrate their 2025 Goalkeepers nominees – people recognised for accelerating real progress. One of them was Ugandan entomologist Krystal Birungi, who is working on one of the the next frontiers of malaria solutions: developing genetically modified mosquitoes to reduce transmission.
My conversation with her, coming just as I was finishing the final edits, reminded me that science never stands still. In her circles, the vaccine had already moved into the rearview mirror. It was a reminder that the story of fighting malaria was one of overlapping interventions; one tool serving as a placeholder until the next one comes along.
Why the vaccine matters
A blueprint for progress
Looking back, it’s incredible how much happened while we were creating this thing. I moved house, Teresa moved countries. Gus had his third child, Anthony found out he was expecting his first. None of us walked out the same people we walked in, and in many strange ways, the making mirrored the story we were telling. There were roadblocks, unexpected challenges, and many, many moments where I was completely humbled by the sheer awesomeness and tenacity of human beings.
Was it successful? Well, that depends on who you’re asking.
In June 2025, Gavi raised $9 billion - far better than expected given the withdrawal of the United States, and enough to fully vaccinate an additional 50 million children by the end of this decade. As of November 2025, more than 40 million doses have already been delivered, with 24 African countries now integrating malaria vaccination into routine immunisation. And, just days ago, Gavi and UNICEF announced a new pricing deal that will secure a further 30 million doses over the next five years. The funding is there. The vaccines are moving.
As for us well, we put everything we had into this series. Our small team worked hours that far outweighed the compensation, there were no egos, and the hardest decisions were always made with generosity. I’m really proud of what we created, and it’s given us the confidence to back ourselves the next time we take on something this big. In terms of audience numbers and downloads though, we haven’t broken any records. Getting people to listen to a good news story about malaria is still a tough sell.
Would we do it again?
I think this podcast fundamentally changed our work at Fix the News. We now have a deep-seated understanding that inside every story we share there’s an entire world made up of invisible chains of people. It’s given us a blueprint for how major developments happen in healthcare, conservation and human rights. It completely unlocked the idea of hidden progress - if none of us can see the full outlines of a story this big and impactful, what else is hiding in plain sight?
So much of the production played out against a backdrop of global uncertainty and devastating funding cuts to aid, and yet everyone we spoke to on the ground was telling us how things were working. About how a disease that’s killed more humans than any other in our history is being pushed back, one child at a time. It was the antidote I didn’t know I needed, and something I definitely didn’t expect from 2025.
Mostly, it’s reaffirmed my faith in the possibility that things can get better. If humanity can pull this off - against a deadly shape-shifting parasite, cultural barriers, funding cuts, systemic challenges, poverty, and an almost century-long timeline – then really, there’s nothing we can’t do.
I guess the only question remaining is, what story should we tackle next?





This is utterly amazing and thrilling to read. Thank you for your tenacity, your commitment to healing the world and your dedication to authenticity. What a testament to community that can enable big changes for the benefit of all.
And, by the way, I listened to the entire series.
Carol Stevenson Seller, PEI. CANADA
Thanks so much for sharing this. As an avid podcast listener I often forget the depth of craft and love behind the episodes that accompany me through my day-to-day and I really appreciate the vulnerability it took for you to post this. I hope you’re all able to feel pride and peace, and I look forward to your next story!